About the VIEW Series :
Vascular Interventions. Every Week.
This series brings you real stories and insights into the world of Interventional Radiology—where advanced imaging meets precise, minimally invasive treatment. One condition at a time, one life-changing procedure a week

For patients on dialysis, an Arteriovenous (AV) fistula is nothing short of a lifeline.
Mr. R never missed his dialysis sessions.
Three times a week, without fail, the 58-year-old would walk into the dialysis center with quiet resilience. His arteriovenous (AV) fistula — that little bulge on his left arm — had been faithfully serving him for over two years. It wasn’t just a piece of surgical plumbing; it was his lifeline.
But last Monday was different.
“Sir, the flow is too low. We can’t run dialysis properly,” the Dialysis technician told him.
Mr. R looked down at his arm. The familiar thrill — that faint vibration he used to feel under his fingers — was gone.
Panic set in. Without dialysis, toxins would build up in his body. He would start feeling breathless and swollen. The last time his fistula had clotted, they had to put in a neck catheter. He remembered how uncomfortable and risky that had been. And they had to then create a new AV fistula.
His nephrologist didn’t waste time.
“Go see the Interventional Radiologist. Let’s see if we can salvage this fistula.”
At our Center:
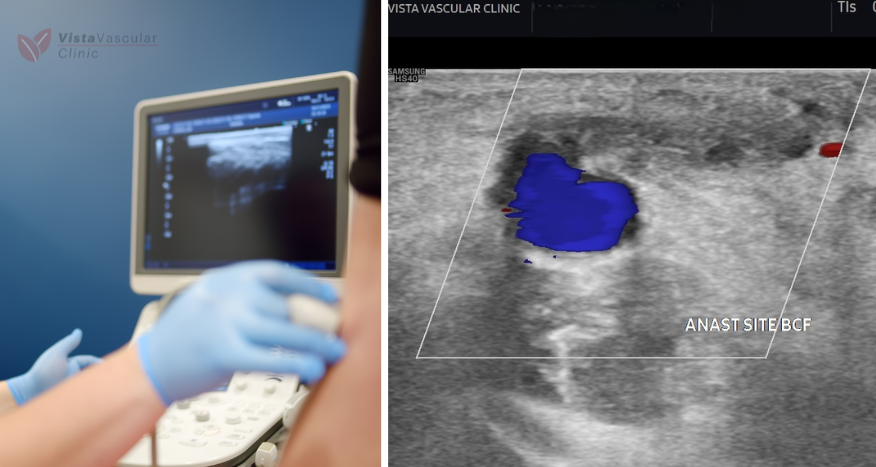
We met Mr. R at our center. He was a little anxious, but quietly hopeful. We performed a Doppler ultrasound at bedside. It didn’t take long to confirm our suspicion — the fistula was completely occluded. No flow. No thrill.
But this didn’t mean the end of the road. We decided to act quickly.
Mr. R was shifted to the angio suite that same afternoon. He remained fully awake — no general anesthesia needed, just local numbing at the access site.
Using fluoroscopy (live X-ray guidance), we navigated a fine catheter into the fistula and injected contrast dye. The vessel lit up like a map, confirming the blockage — a total occlusion at the outflow vein.
“There’s the problem,” I said. “Let’s see if we can bring it back.”
A guidewire was carefully threaded across the blockage — the first critical step. Once we crossed it, we delivered a tiny balloon and gently inflated it at the narrowed segment. No surgery. No stitches. Just precision from within.
Within minutes, we saw it: flow restored. The contrast flowed freely through the vessel, and Mr. R’s fistula had come back to life.

“You should feel that thrill again soon,” I told him. “Let’s get you to the dialysis unit and see how it holds up.”
A little while later, as the dialysis machine hummed and the fistula held steady, Mr. R smiled — a mix of relief and quiet gratitude.
Why This Matters
Mr. R didn’t need another surgery to create a new AV fistula.
He didn’t need a dialysis catheter.
He didn’t miss a single dialysis session.
All because the problem was caught early — and because interventional radiology offers a precise, non-surgical way to restore blocked AV fistulas.
The Takeaway
- If you or a loved one is on dialysis, check the thrill in your fistula daily.
- Report any swelling, sluggish flow, or difficulty during dialysis right away.
- Early referral to an Interventional Radiologist can save your fistula — and prevent hospital stays or complications.
- These procedures are usually day-care, minimally invasive, and highly effective.
Suggested Reading
1. National Kidney Foundation: Hemodialysis Access – what you need to know?https://www.kidney.org/kidney-topics/hemodialysis-access
2. KDOQI (Kidney Disease Outcomes Quality Initiative) Clinical Practice Guideline for Vascular Access: 2019 Update. https://www.ajkd.org/article/S0272-6386(19)31137-0/fulltext